Macular Edema in RVO: How Anti-VEGF Therapy is Changing Visual Outcomes
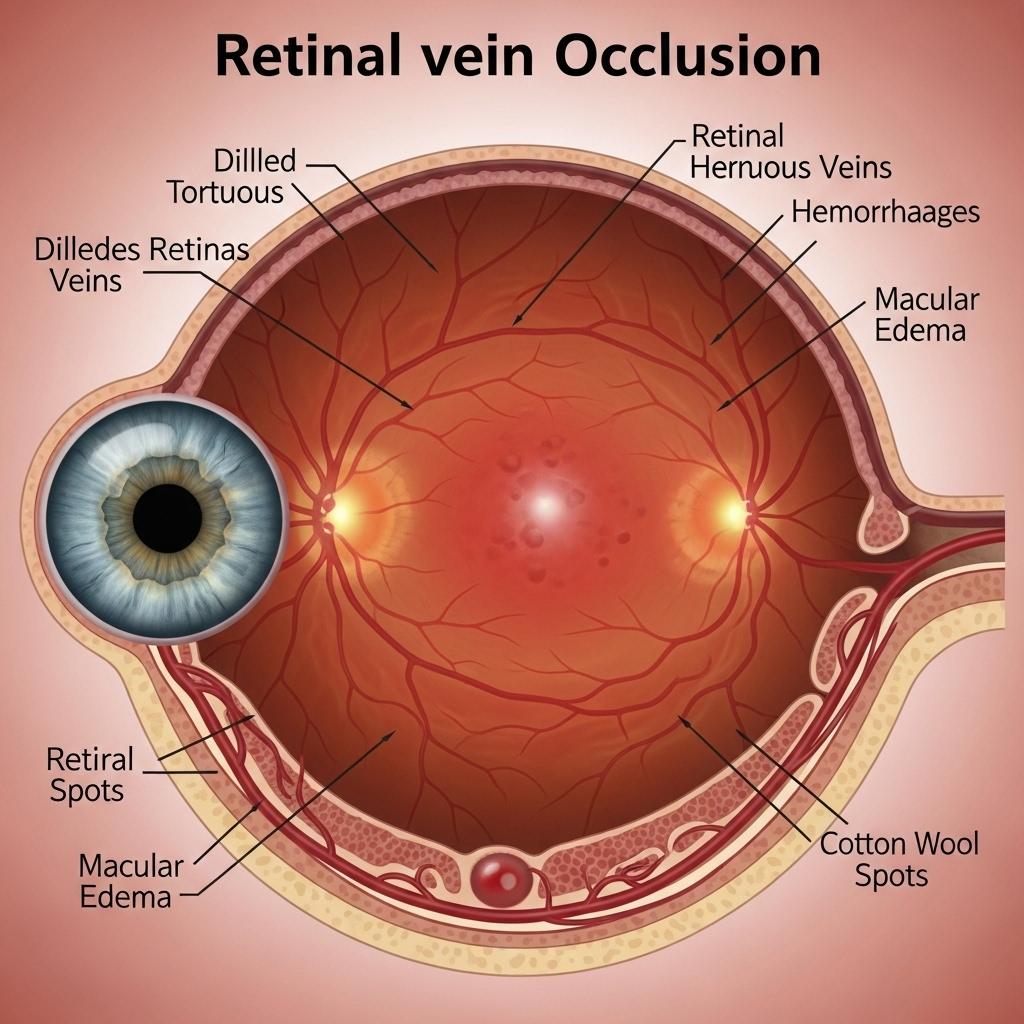
Retinal Vein Occlusion (RVO) is a leading cause of sudden, painless vision loss in middle-aged and older adults. As a vascular disorder of the retina, RVO occurs when a blockage forms in the veins that drain blood from the retina, leading to hemorrhage, edema, and ischemia. With the rise in systemic vascular diseases like hypertension and diabetes, RVO is becoming more prevalent, requiring rapid diagnosis and evolving management strategies.
Request a sample copy of the CI report at: https://www.datamintelligence.com/strategic-insights/ci/retinal-vein-occlusion-rvo
Understanding RVO: Branch vs. Central
RVO is broadly classified into two major types:
1. Central Retinal Vein Occlusion (CRVO): Involves blockage of the central vein at the optic nerve head, often resulting in widespread retinal damage and severe visual impairment.
2. Branch Retinal Vein Occlusion (BRVO): Affects smaller branches of the retinal vein, typically in one quadrant of the retina. BRVO is more common and generally has a better visual prognosis than CRVO.
Both types result in venous congestion, retinal hemorrhages, cotton-wool spots, and fluid leakage that may affect the macula.
Risk Factors and Comorbidities
RVO is closely associated with systemic conditions, especially in individuals over 50.
Major risk factors include:
* Hypertension (most common)
* Diabetes mellitus
* Hyperlipidemia
* Glaucoma
* Smoking
* Thrombophilic disorders (e.g., protein C/S deficiency, antiphospholipid syndrome)
A complete systemic evaluation is critical for patients presenting with RVO to manage underlying vascular risk factors.
Pathophysiology and Complications
The retinal vein becomes occluded typically due to compression from adjacent atheroscl*** arteries, hypercoagulable states, or inflammatory processes. This leads to stagnation of blood flow, increased venous pressure, and leakage of blood and fluid into the retina.
Key complications include:
* Macular edema, the most common cause of vision loss
* Neovascularization, may result in neovascular glaucoma or vitreous hemorrhage
* Retinal ischemia, especially in CRVO, increases the risk of irreversible vision damage
Diagnostic Approach
Diagnosis of RVO is typically clinical, supported by:
* Fundus photography – reveals retinal hemorrhages and vein dilatation
* Optical coherence tomography (OCT): evaluates macular edema
* Fluorescein angiography: assesses retinal perfusion and neovascularization
* OCT-Angiography (OCT-A): a non-invasive tool gaining popularity in RVO imaging
These tools also aid in treatment planning and response monitoring.
Current Treatment Landscape
The treatment of RVO is primarily focused on managing complications such as macular edema and neovascularization:
* Anti-VEGF Therapy
Intravitreal anti-VEGF agents (e.g., ranibizumab, aflibercept, bevacizumab) are the mainstay of treatment.
These agents reduce vascular permeability and edema, improving vision in a majority of patients with CRVO and BRVO.
* Corticosteroid Implants
Dexamethasone implants (Ozurdex) are approved for RVO-related macular edema, particularly in patients not responding to anti-VEGF therapy.
Side effects include elevated intraocular pressure and cataract progression.
* Laser Photocoagulation
Historically used in BRVO, laser photocoagulation is now reserved for treating neovascularization and non-resolving cases in conjunction with pharmacologic therapy.
Emerging Therapies and Long-Term Outlook
Research into sustained-release delivery systems and combination therapies is ongoing. Port delivery systems, gene therapy targeting VEGF pathways, and longer-acting anti-inflammatory agents are being explored. Personalized therapy based on perfusion status and biomarkers is likely to shape the next phase of RVO care.
Request a CI consultation at:
https://www.datamintelligence.com/strategic-insights/ci/retinal-vein-occlusion-rvo
Importance of Systemic Control and Follow-Up
Effective RVO management includes addressing systemic risk factors to prevent recurrence or involvement of the fellow eye. Patients should undergo regular blood pressure and glucose monitoring, lipid management, and thrombophilia screening where indicated.
Long-term ophthalmologic follow-up is essential, especially in ischemic RVO, where complications may develop even after initial treatment success.
About DataM Intelligence
DataM Intelligence 4Market Research LLP delivers real-time competitive intelligence across autoimmune, immunologic, ophthalmic, and rare disease domains. Our insights span clinical pipelines, regulatory milestones, and commercialization strategies to support global healthcare stakeholders.
🔗 Visit: www.datamintelligence.com
- Art
- Causes
- Crafts
- Dance
- Drinks
- Film
- Fitness
- Food
- Spellen
- Gardening
- Health
- Home
- Literature
- Music
- Networking
- Other
- Party
- Religion
- Shopping
- Sports
- Theater
- Wellness


