Patrocinado
New Horizons in Celiac Disease: From Gut Health to Gene Therapy
Celiac disease is no longer viewed as a simple dietary intolerance. It is now recognized as a complex autoimmune disorder triggered by the ingestion of gluten in genetically predisposed individuals. Affecting approximately 1% of the global population, celiac disease often goes undiagnosed or misdiagnosed due to its wide range of gastrointestinal and extraintestinal manifestations. However, diagnostics, biomarkers, and gluten-free food regulation advances are rapidly transforming the clinical landscape.
Request a sample copy of the CI report at: https://www.datamintelligence.com/download-sample/celiac-disease-***s-market
Understanding Celiac Disease and Its Pathogenesis
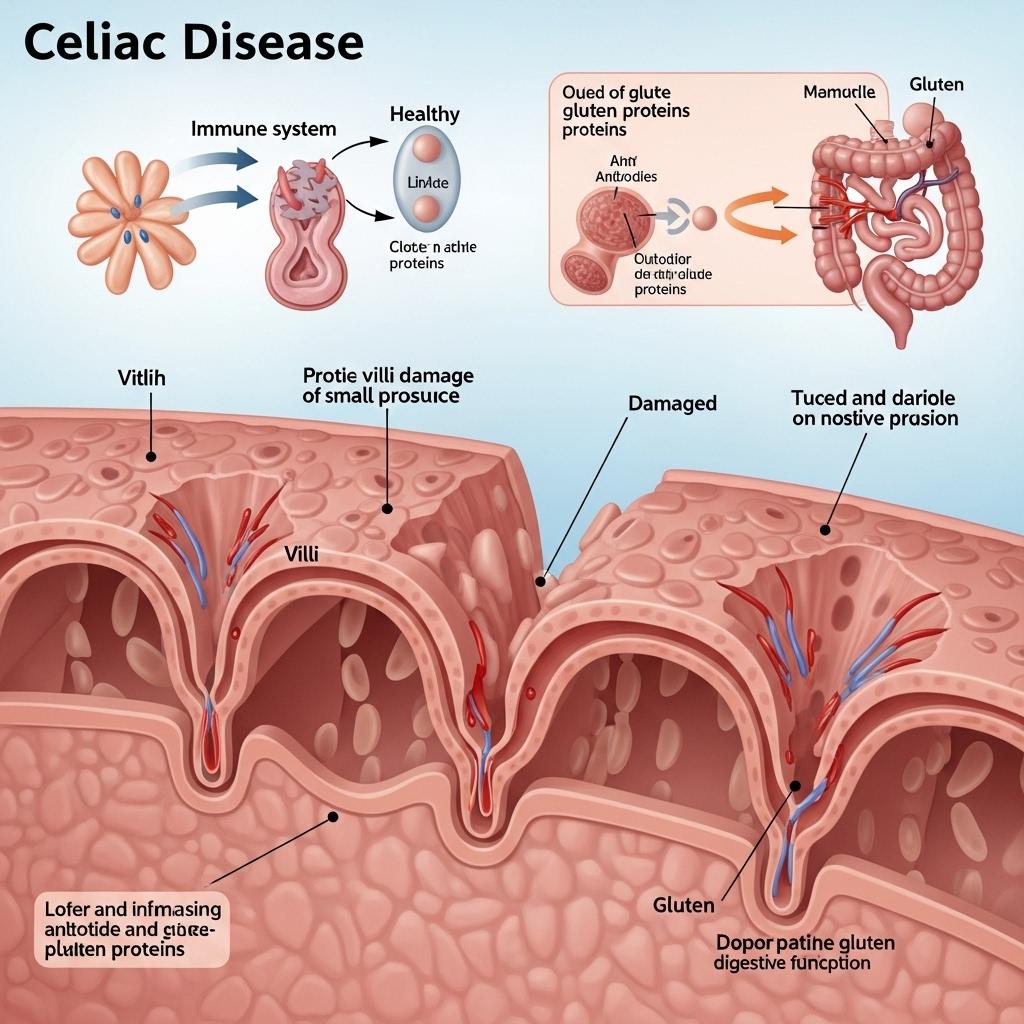
Celiac disease is driven by an immune reaction to gluten, a protein found in wheat, barley, and rye. In affected individuals, gluten triggers an inflammatory response that damages the small intestine’s villi—tiny structures responsible for nutrient absorption. The result is malabsorption, leading to symptoms such as chronic diarrhea, weight loss, bloating, and fatigue. Extraintestinal signs like anemia, dermatitis herpetiformis, infertility, and neurologic issues also complicate diagnosis.
Celiac disease is strongly associated with HLA-DQ2 and HLA-DQ8 genotypes, though not all individuals with these genes develop the condition. This underscores the interplay between genetic predisposition and environmental triggers.
Diagnostic Evolution: From Biopsy to Serologic Precision
Traditionally, diagnosis required an intestinal biopsy to confirm villous atrophy. Today, highly specific and sensitive serologic markers—such as tissue transglutaminase IgA (tTG-IgA) and endomysial antibodies (EMA)—allow for noninvasive diagnosis, especially in symptomatic patients. Anti-deamidated gliadin peptide (DGP) antibodies and genetic testing for HLA-DQ2/DQ8 are also used in ambiguous cases.
In pediatric populations, serology may even eliminate the need for biopsy, enabling earlier diagnosis and management. Improved screening practices are helping uncover silent and atypical forms of the disease, especially in high-risk groups such as first-degree relatives, type 1 diabetics, and patients with autoimmune thyroiditis.
Gluten-Free Diet: Foundation, Not the Finish Line
The cornerstone of celiac disease management remains strict, lifelong adherence to a gluten-free diet (GFD). For most patients, a GFD leads to mucosal healing and symptom resolution. However, adherence challenges persist due to social, cultural, and economic factors. Even trace gluten exposure can lead to relapse or persistent symptoms.
Regulatory oversight has improved access to certified gluten-free products, yet cross-contamination remains a concern in restaurants and food processing. Apps, support groups, and dietitian-guided counseling have become crucial tools for maintaining compliance.
Non-Dietary Therapies: A New Era of Innovation
Despite best efforts, up to 30% of patients experience non-responsive or refractory celiac disease. This has led to the development of non-dietary therapeutic candidates, aiming to protect or restore the gut barrier, degrade gluten peptides, or modulate the immune response.
Investigational approaches include:
* Larazotide acetate: Enhances tight junction integrity to reduce intestinal permeability.
* Nexvax2 and other peptide-based immunotherapies: Attempt to induce immune tolerance to gluten.
* Enzyme therapies: ***gned to break down gluten in the stomach before it reaches the small intestine.
Though not yet approved, these therapies offer hope for those with persistent symptoms or accidental gluten exposure.
Challenges and Future Perspectives
* Celiac disease management still faces hurdles:
* Delayed diagnosis due to variable presentations.
* Inconsistent GFD access and labeling standards worldwide.
* Lack of therapeutic options for refractory cases.
Emerging research is exploring the gut microbiome’s role in disease modulation, genetic biomarkers for response prediction, and digital tools for real-time diet tracking. In the long term, a personalized medicine approach may help stratify patients by risk, symptom severity, and therapeutic needs.
Read the full CI Insights report: https://www.datamintelligence.com/strategic-insights/celiac-disease
Conclusion: From Awareness to Action
Celiac disease care is transforming—from reactionary diagnosis to proactive screening and from dietary control to immunologic precision. With a growing toolkit of diagnostics, patient support systems, and pipeline therapies, the future holds promise for more sustainable disease control and improved quality of life. Multidisciplinary care and continued innovation will be key to redefining the standard of care for this lifelong condition.
About DataM Intelligence
DataM Intelligence 4Market Research LLP delivers real-time competitive intelligence across autoimmune, immunologic, and rare disease spaces. Our insights span clinical pipelines, regulatory benchmarks, and commercialization strategies for stakeholders in global life sciences.
🔗 Visit: www.datamintelligence.com