Mental Health Billing Services
Mental Health Billing Services: Streamlining Revenue for Mental Health Providers
Introduction
Managing the financial side of a mental health practice can be challenging. From insurance claim denials to complex billing codes, administrative burdens can distract providers from focusing on patient care. Our mental health billing services are designed to simplify the revenue cycle, reduce errors, and ensure timely reimbursements, helping your practice run efficiently and profitably.
What Are Mental Health Billing Services?
Mental health billing services involve handling all aspects of billing and claims management for mental health providers, including psychiatrists, psychologists, therapists, and counselors. These services typically include:
Claims submission and follow-up
Patient billing and statements
Insurance verification
Denial management and appeals
Detailed reporting and account reconciliation
By outsourcing these tasks to experts, mental health providers can focus on delivering quality care while ensuring financial accuracy and compliance.
Key Benefits of Mental Health Billing Services
1. Accurate Claims Submission
Billing for mental health services often involves complex coding systems like CPT and ICD-10. Our services ensure that all claims are coded correctly, reducing the risk of denials and delayed payments.
2. Faster Reimbursements
Timely submission of accurate claims helps mental health providers receive reimbursements faster. Our team tracks claims from submission to payment, ensuring no revenue is lost due to delays or errors.
3. Reduced Denials and Errors
Errors in billing can lead to claim denials and lost revenue. We proactively identify and correct potential errors, helping your practice minimize denials and improve financial performance.
4. Compliance with Regulations
Healthcare billing is subject to strict regulations, including HIPAA and payer-specific rules. Mental Health Billing Services ensures that all billing processes comply with these standards, reducing audit risks.
5. Enhanced Reporting and Transparency
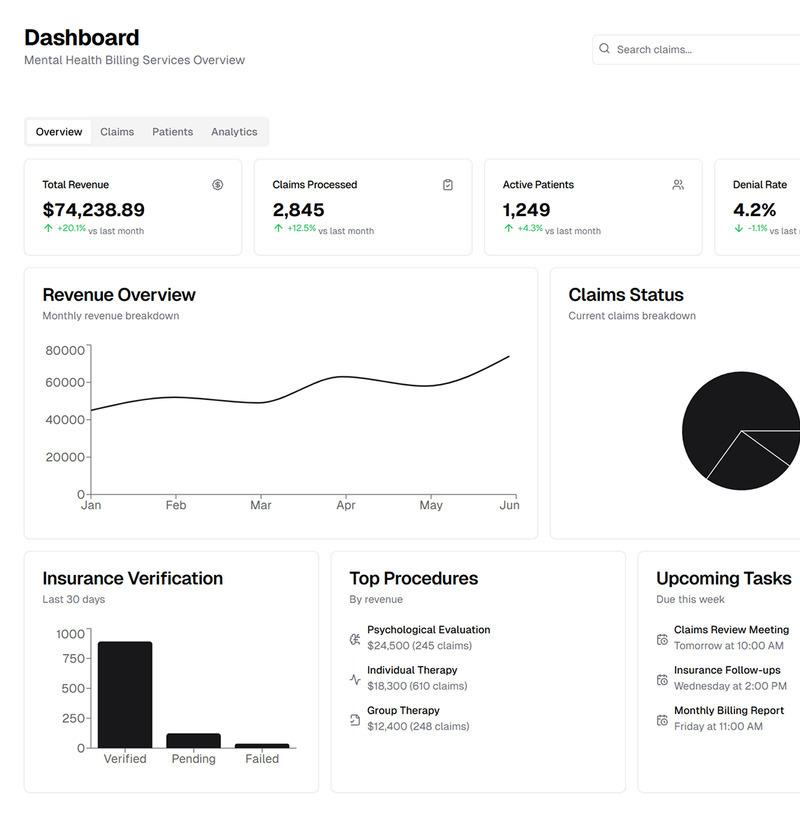
Our services include detailed reports on billing, collections, and account status. This transparency helps providers make informed financial decisions and plan for growth.
How Our Mental Health Billing Services Work
Patient Registration & Verification:
We begin by verifying patient insurance details and eligibility to prevent claim rejections.
Coding & Claim Preparation:
Using accurate CPT and ICD-10 codes, we prepare claims to meet payer requirements.
Claims Submission & Follow-Up:
Claims are submitted electronically or manually as required, and we follow up on any pending or denied claims.
Patient Billing & Collections:
We handle patient statements, payment plans, and collections while maintaining a professional and patient-friendly approach.
Reporting & Analysis:
Providers receive regular reports on claim status, revenue trends, and account discrepancies, helping optimize financial management.
Why Choose Us?
Expert Team: Our billing specialists have extensive experience in mental health billing.
Custom Solutions: Services are tailored to meet the unique needs of your practice.
Technology-Driven: We use advanced billing software for accuracy and efficiency.
Focus on Care: By handling billing, we allow providers to focus on what matters most—patient care.
Conclusion
Efficient revenue cycle management is critical for mental health practices. Our mental health billing services reduce administrative burdens, ensure compliance, and maximize revenue, allowing providers to focus on delivering quality care. Partner with us to streamline your billing process and maintain financial stability.
- Art
- Causes
- Crafts
- Dance
- Drinks
- Film
- Fitness
- Food
- Spiele
- Gardening
- Health
- Startseite
- Literature
- Music
- Networking
- Andere
- Party
- Religion
- Shopping
- Sports
- Theater
- Wellness


