Understanding the Pathogenesis of Inflammatory Bowel Disease
Inflammatory Bowel Disease (IBD) encompasses two major chronic autoimmune conditions. Crohn’s disease (CD) and ulcerative colitis (UC) are characterized by intestinal inflammation, relapsing symptoms, and systemic immune dysregulation. Affecting over 10 million people worldwide, IBD leads to impaired quality of life, recurrent hospitalizations, and long-term complications if not managed early and effectively.
Fueled by a deeper understanding of mucosal immunology and microbiome interactions, IBD treatment has rapidly evolved beyond symptom control to targeted, biologic, and small molecule-based therapies offering durable remission and mucosal healing.
Request a sample copy of the CI report at: https://www.datamintelligence.com/download-sample/inflammatory-bowel-disease-market
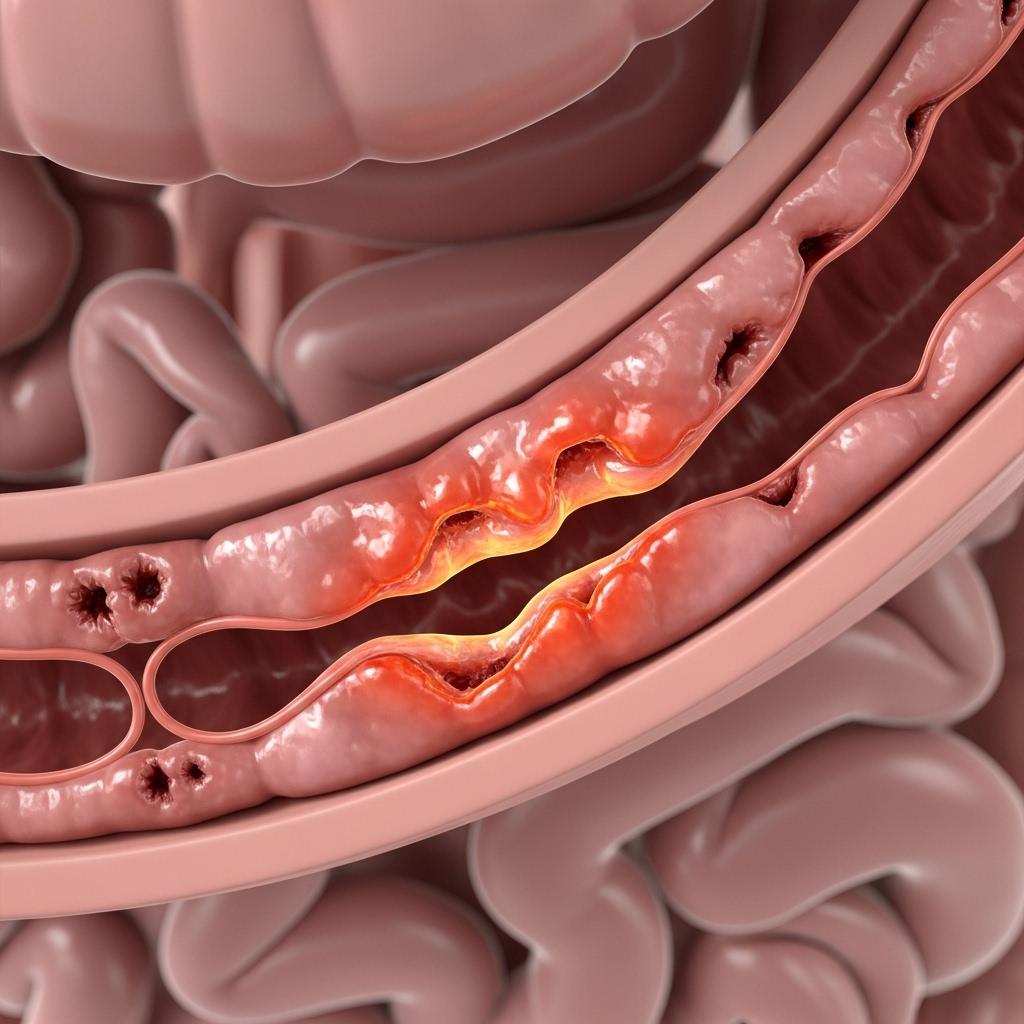
IBD Pathogenesis: The Immune System in Overdrive
IBD is caused by an inappropriate immune response to gut microbiota in genetically predisposed individuals. Environmental triggers, such as diet, antibiotics, smoking, and stress, may disrupt intestinal homeostasis, leading to:
* Chronic mucosal inflammation
* Breakdown of epithelial barrier integrity
* Dysbiosis of gut microbiota
* Excess production of proinflammatory cytokines (TNF-α, IL-12/23)
Crohn’s disease can affect any part of the gastrointestinal tract and is typically transmural and patchy, while ulcerative colitis is limited to the colon and involves continuous mucosal inflammation.
Clinical Manifestations and Diagnosis
IBD symptoms vary based on disease type, location, and severity but commonly include:
1. Abdominal pain and cramping
2. Chronic diarrhea (sometimes bloody)
3. Weight loss and fatigue
4. Fever and urgency
5. Extraintestinal symptoms (arthritis, skin lesions, uveitis)
6. Diagnosis requires a combination of:
7. Colonoscopy with biopsy
8. Stool tests to rule out infections
9. Cross-sectional imaging (MR enterography/CT)
10. Fecal calprotectin as a marker of intestinal inflammation
Early diagnosis and accurate disease classification are key to optimizing treatment and preventing irreversible complications.
Treatment Landscape: Moving Beyond Steroids
The main goal of IBD treatment is inducing and maintaining remission, preventing complications, and enhancing patient quality of life. Treatment is tailored based on disease severity, extent, and response to prior therapies.
Conventional Therapies
1. 5-aminosalicylic acids (5-ASA): First-line in mild-to-moderate UC
2. Corticosteroids: Short-term relief in moderate-to-severe flares
3. Immunomodulators (azathioprine, methotrexate): Steroid-sparing agents
Biologics and Targeted Therapies
1. Anti-TNF agents (infliximab, adalimumab): Proven efficacy in both UC and CD
2. Anti-integrin agents (vedolizumab): Gut-specific with fewer systemic effects
3. Anti-IL-12/23 agents (ustekinumab): Effective for moderate-to-severe CD
4. JAK inhibitors (tofacitinib, upadacitinib): Oral small molecules for UC
Precision Medicine in IBD
The growing focus on precision IBD care aims to use patient-specific markers, genetic variants, and microbiome profiles to guide therapy selection and predict response.
Key trends include:
1. Therapeutic *** monitoring (TDM) for optimizing biologic dosing
2. Biomarkers (e.g., calprotectin, CRP) for early detection of relapse
3. Non-invasive imaging for disease monitoring
4. Microbiome-based therapies and fecal microbiota transplantation (FMT)
These approaches enhance treatment personalization and minimize long-term immunosuppression.
Complications and Long-Term Management
Uncontrolled IBD can lead to complications such as:
1. Fistulas and strictures in Crohn’s disease
2. Colon cancer risk in long-standing UC
3. Osteoporosis, anemia, and malnutrition
4. Psychosocial stress, depression, and anxiety
A multidisciplinary approach involving gastroenterologists, dietitians, psychologists, and colorectal surgeons is essential for holistic management. Regular surveillance colonoscopies and lifestyle counseling are critical components of long-term care.
Read the full CI Insights report: https://www.datamintelligence.com/strategic-insights/inflammatory-bowel-disease-ibd
Unmet Needs and Future Outlook
Despite therapeutic advances, many patients continue to experience partial response, intolerance, or loss of efficacy over time.
Key unmet needs include:
1. Earlier diagnosis in underserved areas
2. Non-invasive diagnostics with higher specificity
3. Affordable access to biosimilars and novel agents
4. Better treatment options for pediatric and refractory cases
Research into next-generation biologics, oral agents, and gene therapy continues to accelerate. With increasing focus on treat-to-target strategies, achieving deep remission and mucosal healing is now a realistic goal for many patients.
About DataM Intelligence
DataM Intelligence 4Market Research LLP delivers real-time competitive intelligence across autoimmune, immunologic, and rare disease spaces. Our insights span clinical pipelines, regulatory benchmarks, and commercialization strategies for stakeholders in global life sciences.
🔗 Visit: www.datamintelligence.com
- Art
- Causes
- Crafts
- Dance
- Drinks
- Film
- Fitness
- Food
- Jogos
- Gardening
- Health
- Início
- Literature
- Music
- Networking
- Outro
- Party
- Religion
- Shopping
- Sports
- Theater
- Wellness


