From Misery to Management: New Hope for Prurigo Nodularis Patients
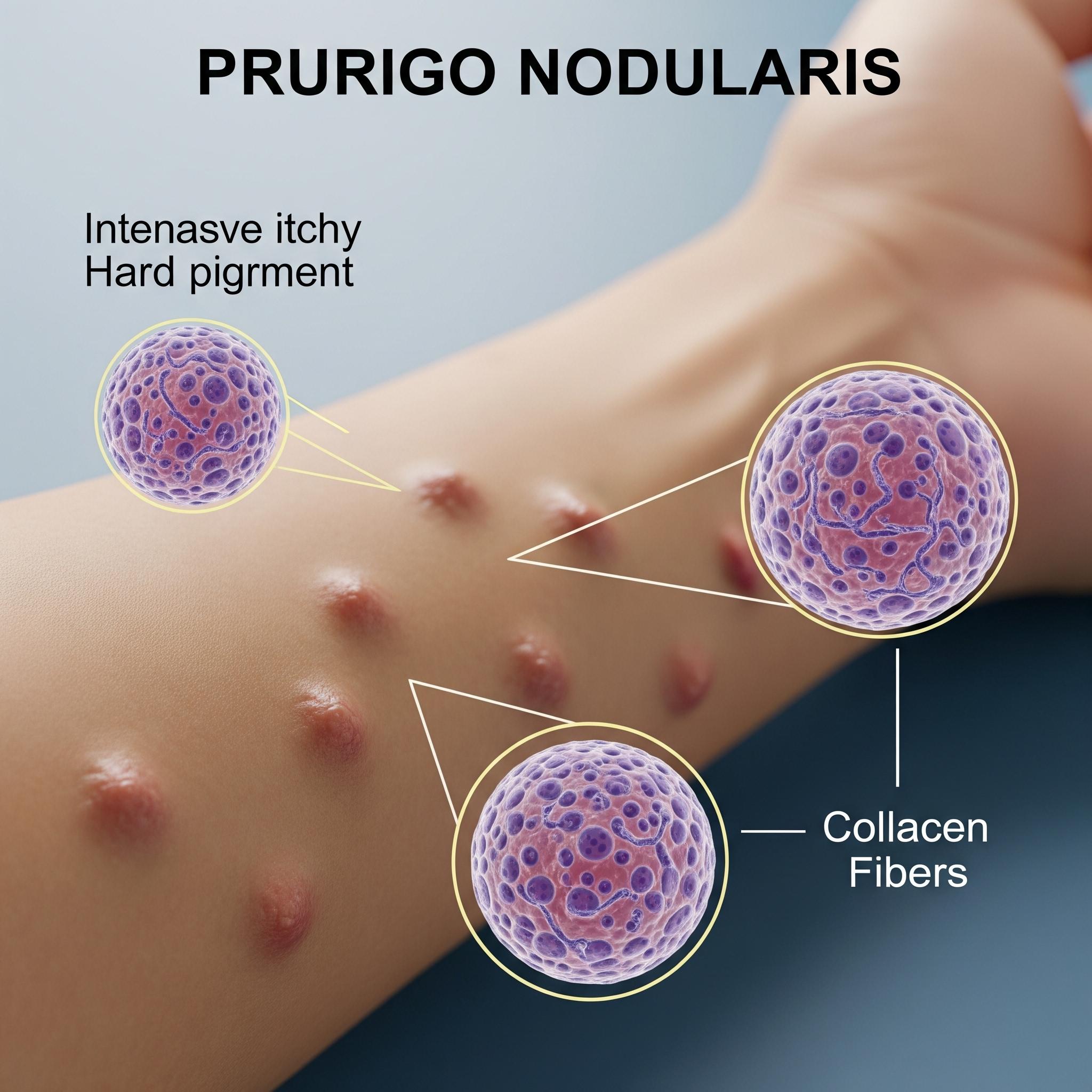
Prurigo Nodularis (PN) is a chronic inflammatory skin disorder marked by intensely itchy nodules, often resulting in skin damage from constant scratching. Once considered a dermatologic mystery with limited treatment options, PN is now gaining clinical and therapeutic momentum due to its complex immunological profile. As novel biologics reshape inflammatory skin disease treatment, PN is emerging as a priority condition in dermatology innovation.
Request a sample copy of the CI report at:
https://www.datamintelligence.com/download-sample/prurigo-nodularis-treatment-market
What Is Prurigo Nodularis?
PN is characterized by multiple, firm, hyperkeratotic nodules typically appearing on the arms, legs, and trunk. These lesions develop in response to chronic scratching and are accompanied by persistent, severe pruritus. The itch-scratch cycle drives both physical and psychological distress, often leading to sleep disturbance, anxiety, and depression.
The disease most commonly affects:
* ***s aged 40–70
* Patients with atopic dermatitis or systemic pruritus
* Individuals with metabolic syndrome, diabetes, or chronic kidney disease
The condition is chronic, relapsing, and often resistant to conventional therapies.
Immunopathogenesis and Triggers
PN is now understood to be driven by neuroimmune dysregulation, with a central role played by type 2 inflammation. Interleukins IL-4, IL-13, and IL-31 contribute to nerve fiber hypersensitivity and immune-mediated skin inflammation.
Common contributing factors include:
* Atopic diathesis
* Chronic systemic diseases (e.g., liver, kidney failure)
* Neuropathies
* Psychiatric comorbidities
* Infections (e.g., HIV, hepatitis C)
This insight has opened the door to precision-targeted therapies rather than broad immunosuppression.
Diagnostic Clarity and Differentiation
Diagnosis of PN is clinical, based on:
* Presence of multiple nodules with excoriation or crusting
* History of chronic itching lasting ≥6 weeks
* Exclusion of mimics like lichen simplex chronicus, bullous pemphigoid, or cutaneous lymphoma
Skin biopsy is not always necessary but can confirm hypertrophic lichenification and eosinophilic infiltration. Workups may include blood tests, imaging, or patch testing depending on systemic involvement.
Traditional Management: Limited and Non-Specific
Conventional treatments for PN aim to control itch and inflammation but often fall short in refractory cases. Common therapies include:
* Topical corticosteroids or calcineurin inhibitors
* Antihistamines (limited effectiveness)
* Gabapentin or pregabalin for neuropathic itch
* Phototherapy (NB-UVB)
* Systemic immunosuppressants (e.g., methotrexate, cyclosporine)
However, side effects, limited efficacy, and recurrence after withdrawal remain key challenges.
Breakthrough Therapies: Biologic Agents Redefine Control
Recent biologic approvals are changing the treatment landscape by targeting the key cytokines responsible for chronic itch and inflammation.
Notable Approvals and Advancements:
* Dupilumab (Dupixent): IL-4Rα antagonist blocking IL-4 and IL-13 signaling; first FDA-approved biologic for PN (2022), showing rapid itch relief and nodule reduction.
* Nemolizumab: IL-31 receptor antagonist under investigation, demonstrating promising results in reducing pruritus intensity.
These agents offer targeted control without the long-term toxicity associated with steroids or systemic immunosuppressants.
Holistic Care and Long-Term Support
Management of PN extends beyond pharmacology. Key supportive strategies include:
* Behavioral therapy to break the itch-scratch cycle
* Emollient-based skincare regimens
* Mental health support for anxiety and depression
* Avoidance of irritants and allergens
Dermatologists often work with neurologists, allergists, and psychiatrists in multidisciplinary care.
Unmet Needs and Future Directions
Despite biologic advancements, PN remains underdiagnosed and undertreated. Major gaps include:
* Lack of disease awareness in primary care
* Delayed specialist referral
* Limited access to biologics in low-resource settings
* Need for long-term real-world data on treatment durability
Ongoing trials are exploring JAK inhibitors, monoclonal antibodies, and novel neuromodulators.
Read the full CI Insights report:
https://www.datamintelligence.com/strategic-insights/prurigo-nodularis-pn
Conclusion: A New Era for Prurigo Nodularis
Prurigo Nodularis is transitioning from a neglected dermatologic condition to a model for neuroimmune-targeted care. With biologics like dupilumab leading the way, patients now have hope for lasting relief, improved sleep, and restored quality of life. The next step is ensuring early diagnosis, broad access, and continued innovation to meet the complex needs of PN patients worldwide.
About DataM Intelligence
DataM Intelligence 4Market Research LLP is a global provider of competitive insights and real-time ***ytics across immunology, dermatology, and rare disease sectors. Our reports track emerging therapies, clinical trials, market trends, and access dynamics.
🔗 Visit: www.datamintelligence.com
- Art
- Causes
- Crafts
- Dance
- Drinks
- Film
- Fitness
- Food
- Games
- Gardening
- Health
- Home
- Literature
- Music
- Networking
- Other
- Party
- Religion
- Shopping
- Sports
- Theater
- Wellness


