Navigating Dermatomyositis: Early Signs, Risk Factors, and Long-Term Outlook
Dermatomyositis (DM) is a rare autoimmune disorder that bridges dermatology and neuromuscular medicine. Marked by chronic inflammation of the skin and skeletal muscles, it presents with characteristic rashes and progressive muscle weakness. As diagnostic techniques and immunotherapies evolve, dermatomyositis is entering a new era of precision medicine, bringing hope to patients who once faced significant disability and diagnostic delays.
Request a sample copy of the CI report at:
https://www.datamintelligence.com/download-sample/juvenile-dermatomyositis-treatment-market
What Is Dermatomyositis?
Dermatomyositis is an idiopathic inflammatory myopathy (IIM) believed to be driven by immune-mediated vascular injury. The condition can occur in both adults and children (juvenile dermatomyositis), and is more common in women.
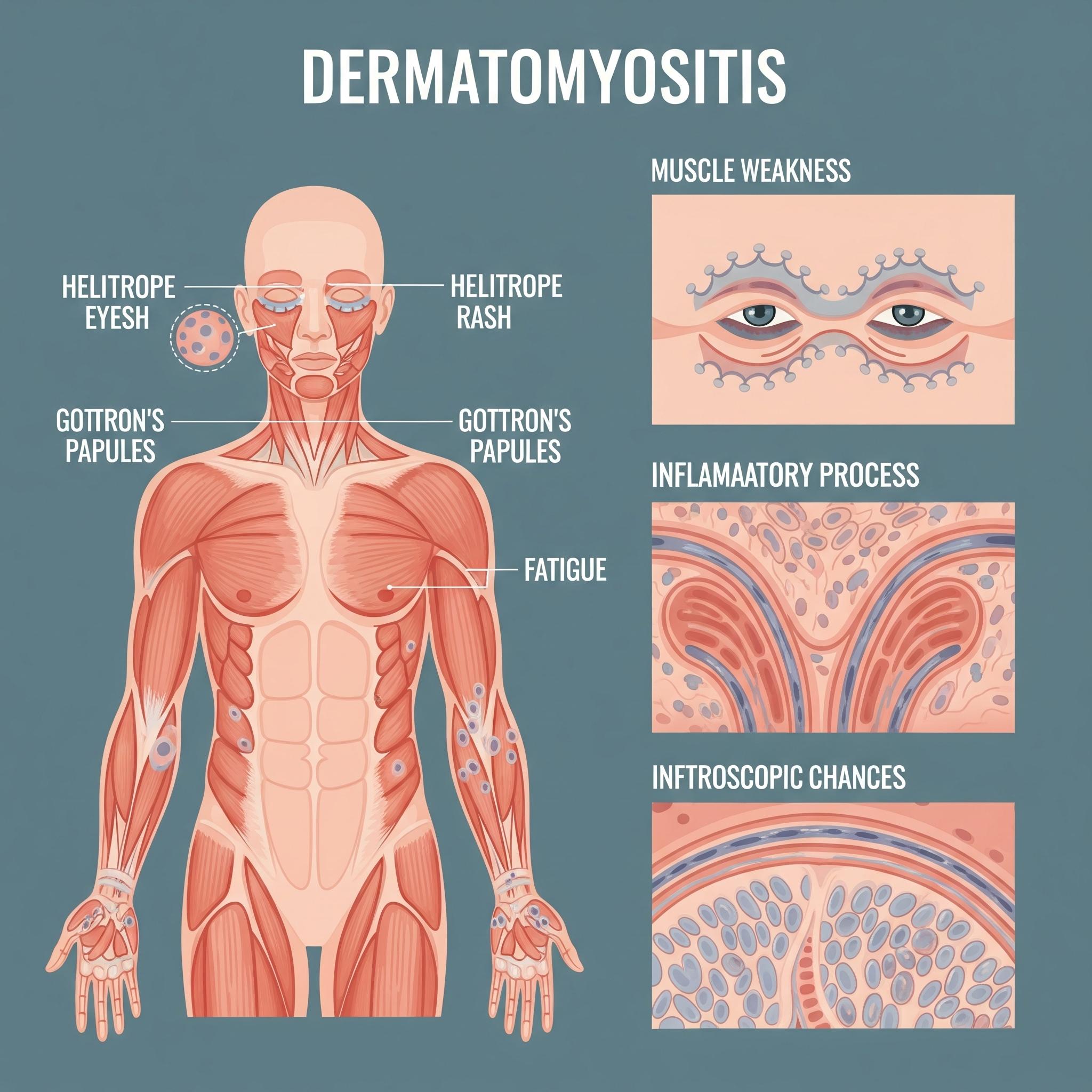
The hallmark symptoms include:
* Symmetric proximal muscle weakness (e.g., hips, shoulders)
* Heliotrope rash (purplish eyelid discoloration)
* Gottron's papules (scaly red patches over joints)
* Fatigue, dysphagia, and photosensitivity
In some cases, interstitial lung disease (ILD), myocarditis, or malignancies may co-exist, especially in adult-onset cases.
Diagnosis and Biomarker-Based Classification
Early and accurate diagnosis is essential to prevent long-term morbidity. Diagnosis involves:
* Elevated creatine kinase (CK) and other muscle enzymes
* Electromyography (EMG)
* Muscle biopsy showing perifascicular atrophy
* Autoantibody testing (e.g., anti-Mi-2, anti-MDA5, anti-TIF1γ)
Anti-MDA5 antibodies, in particular, are associated with rapidly progressive ILD and require aggressive treatment.
Skin biopsy may aid diagnosis when muscle symptoms are minimal, as in clinically amyopathic dermatomyositis (CADM).
First-Line and Steroid-Sparing Treatment Approaches
Corticosteroids (e.g., prednisone) remain the first-line therapy and often lead to initial improvement in strength and rash. However, long-term use brings risks such as:
* Osteoporosis
* Glucose intolerance
* Hypertension
* Muscle atrophy
To reduce steroid dependence, immunosuppressants are commonly introduced, including:
* Methotrexate
* Azathioprine
* Mycophenolate mofetil
For skin-dominant disease, hydroxychloroquine or topical therapies may help manage rashes.
Biologic Therapies and Novel Immunomodulators
Patients with refractory disease or ILD may benefit from targeted biologics. These include:
* Rituximab (anti-CD20 monoclonal antibody): particularly effective in antibody-positive DM
* IVIG (intravenous immunoglobulin): used for resistant skin and muscle disease
* JAK inhibitors (e.g., tofacitinib): under investigation for refractory dermatomyositis with promising anti-inflammatory results
Anti-MDA5-positive patients with ILD often require early combination therapy to prevent respiratory failure.
Cancer Screening and Malignancy Association
Dermatomyositis is a paraneoplastic syndrome in 15–25% of adult cases. Associated cancers include:
* Ovarian
* Breast
* Lung
* Gastric
* Pancreatic
Comprehensive cancer screening at diagnosis and annually thereafter is crucial in adults, particularly those with anti-TIF1γ antibodies or atypical clinical features.
Patient Monitoring and Long-Term Outlook
Management of DM requires regular monitoring of:
* Muscle strength and function
* Pulmonary symptoms and imaging
* Creatine kinase levels* Patient-reported fatigue and quality of life
Dermatologic follow-up helps track treatment response in skin disease. With early diagnosis and appropriate treatment, many patients achieve disease control or remission. However, some experience chronic weakness, calcinosis, or lung damage.
Challenges in Access and Awareness
Barriers to optimal care include:
* Delays in diagnosis due to nonspecific symptoms
* Limited access to autoantibody panels or specialist care in rural settings
* High cost and off-label status of biologics
Education among general physicians and early referral to rheumatology/dermatology can significantly improve patient outcomes.
Read the full CI Insights report:
Conclusion: A Multidisciplinary Approach for a Complex Autoimmune Disorder
Dermatomyositis is no longer a clinical enigma but a defined autoimmune entity with expanding therapeutic options. Advances in immunology, early cancer detection, and targeted therapy are transforming care for this skin-muscle autoimmune disease. As multidisciplinary strategies and patient-centered care models evolve, dermatomyositis patients can look toward improved outcomes and restored quality of life.
About DataM Intelligence
DataM Intelligence 4Market Research LLP offers actionable competitive intelligence across the autoimmune, oncology, and rare disease landscapes. We support organizations with pipeline tracking, market access insights, and clinical trial ***ytics to enable informed decision-making in fast-evolving therapeutic areas.
🔗 Visit: Market Research, Competitive Intelligence, Consulting | DataM Intelligence
- Art
- Causes
- Crafts
- Dance
- Drinks
- Film
- Fitness
- Food
- Games
- Gardening
- Health
- Home
- Literature
- Music
- Networking
- Other
- Party
- Religion
- Shopping
- Sports
- Theater
- Wellness


